A 57 Y/O MALE WITH FEVER, SOB AND VOMITING
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient-related online learning portfolio and your valuable inputs on the comment box.
Consent and de-identification: The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being conserved entirely. No identifiers shall be revealed throughout this piece of work.
Chief complaints:
A 57 y/o male, farmer by occupation, presented with chief complaints of generalised weakness, cough, shortness of breath, fever, loss of appetite, and vomiting since 5 days.
History of presenting illness:
The patient was apparently asymptomatic 5 days ago,
→ then he developed generalised weakness and was unable to stand or walk
→ cough which is dry (non-productive)
→ shortness of breath which is of grade II - grade III
→ low-grade fever associated with sweating, and not associated with chills or rigors
→ episodes of vomiting after consumption of food, which is non-bilious, non-blood stained, non-projectile, and not associated with abdominal pain
Past history:
The patient is a known case of diabetes since 4 years, treated with unknown medication.
The patient is suffering from pain in the knees and lumbar region from 3 years, and is applying balms for relief.
No h/o hypertension, tuberculosis, epilepsy, asthma
Personal history:
Diet: mixed
Appetite: decreased
Bowel and bladder movements: regular
Sleep: adequate
Addictions: regular alcohol consumption in the past, stopped 10 years ago
Family history:
No significant family history.
General examination:
The patient is conscious, coherent and cooperative, moderately built and nourished, and is well oriented to time, place and person.
Pallor: present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Koilonychia: absent
Pedal edema: absent
Lymphadenopathy: absent
Vitals:
Temperature: afebrile
Respiratory rate: 25/min
Blood pressure: 110/80 mm Hg
Pulse: 105 bpm; rate, rhythm, volume, character normal, no radio-radial delay, no radio-femoral delay
Systemic examination:
Respiratory system:
Inspection:
Shape: symmetrical
No dilated veins, scars, nodules or sinuses present.
JVP is not raised
Palpation:
Trachea: central
No intercostal tenderness
Percussion:
Left side: dullness present
Right side: resonant
Auscultation:
Normal vesicular breath sounds heard
No added sounds
Cardiovascular system:
S1, S2 heard
No murmurs
Gastrointestinal tract:
Abdomen: soft, non-tender, no organomegaly, umbilicus is not everted
Central nervous system:
Patient is conscious
No weakness in the upper limbs
No paresthesias
No sensory disturbances in the lower limb
Lower limb tone, power: normal
Provisional Diagnosis:
Pleural effusion with collapse of left lung
Investigations:
Hemogram
Erythrocyte sedimentation rate
Complete urine examination
Serum creatinine
Serum potassium
Blood sugar - fasting
Post lunch blood sugar
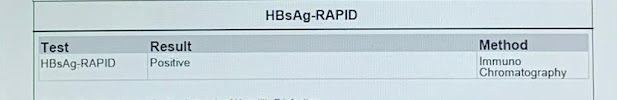
HBsAg - rapid
Liver function tests
Blood urea
Pleural sugar and protein
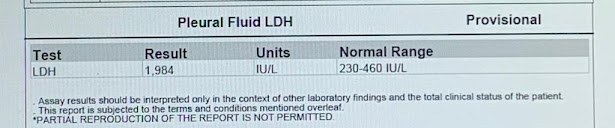
Pleural fluid LDH
LDH
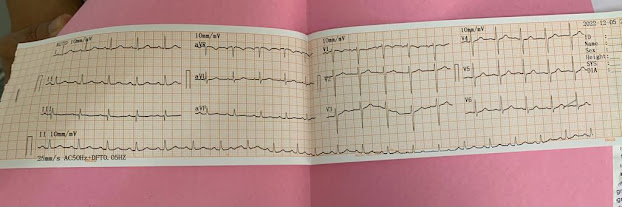
ECG
Doppler 2D echo
USG chest
USG abdomen
Management:
Inj. NEOMOL (if temp > 101° F)
Tab. DOLO 650
Inj. OPTINEURON
Tab. ZOFER
Syp. GRILLINCTUS
GRBS monitoring 6-hourly
Vital charting 4-hourly
Inj. AUGMENTIN


















Comments
Post a Comment